☠️ Approach to Ischemic...

Highlights
- ☠️ Approach to Ischemic Limb Syndromes ☠️
You're in the ICU examining a patient & find a patient with purple discoloration of an extremity concerning for limb ischemia
But the patient has distal pulses!
What's going on? 🧐
Take a journey with me & @OmarosisFugax!
 (View Tweet)
(View Tweet)
- First, when should we be concerned about an Ischemic Limb Syndrome?
Let's keep it simple:
⛳️ Extremity pain (if patient can report)
+
⛳️ Skin changes (eg pallor, purpuric → bullous lesions, blue-discoloration, necrotic changes) (View Tweet)
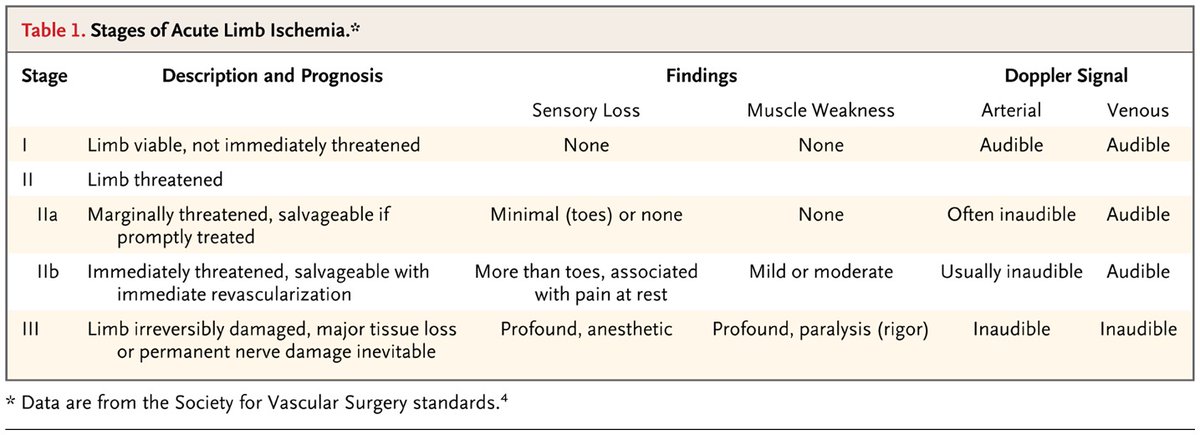
- There are 2 key questions when assessing your patient with an Ischemic Limb Syndrome:
- Pulse/Arterial Doppler? 🤏
If Pulse/Doppler are (–), you're likely dealing with Acute Limb Ischemia (ALI). Remember the P's:
- Pain, Paresthesia, Paralysis
- Pallor, Poikilothermia
 (View Tweet)
(View Tweet)
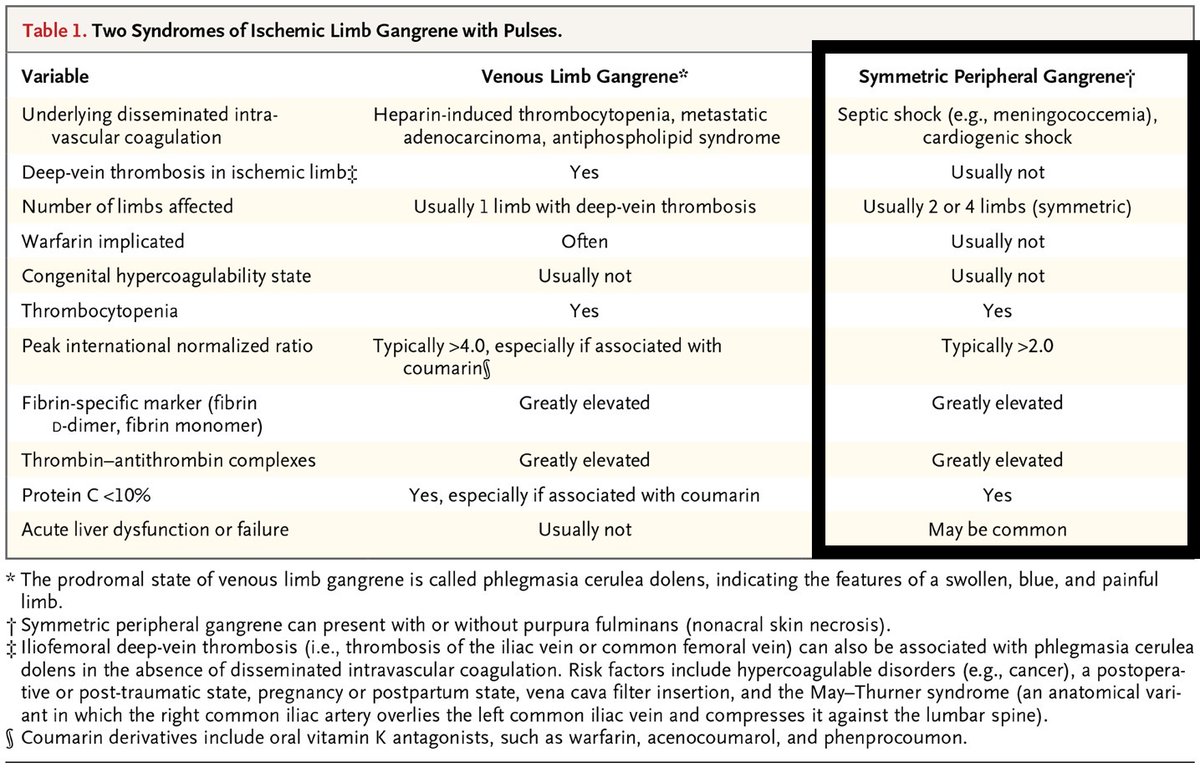
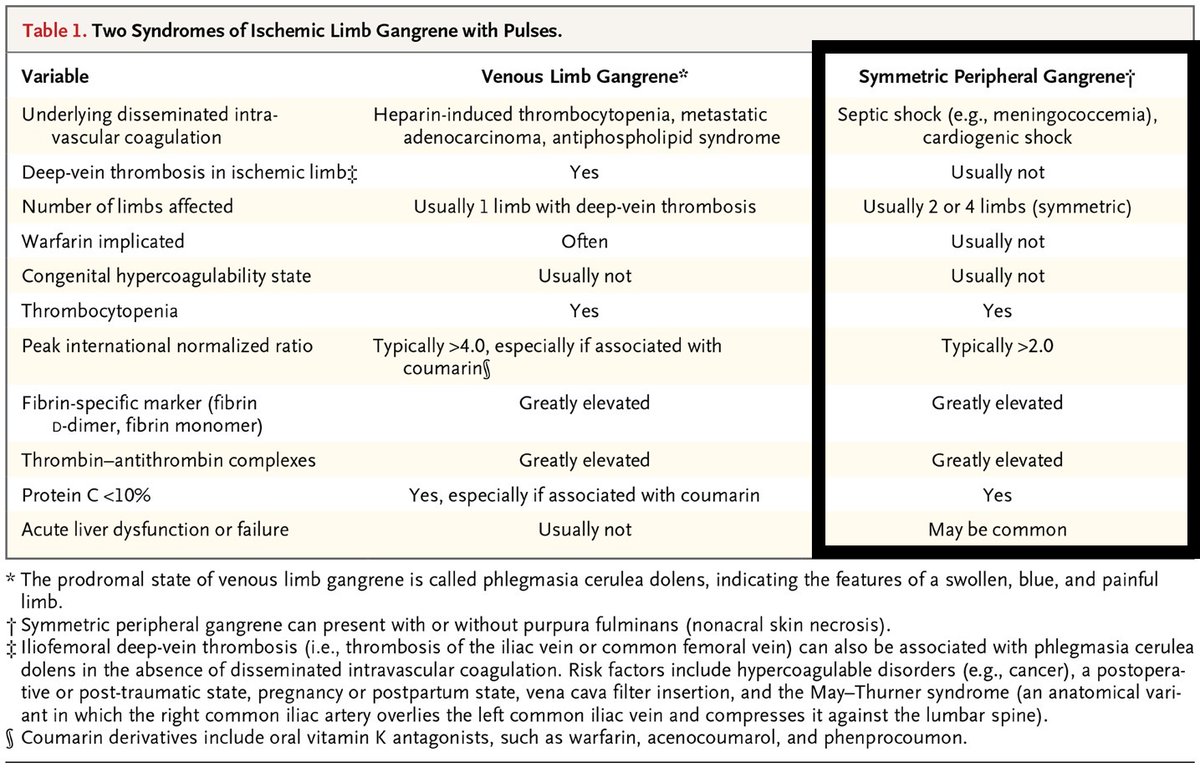
- If Pulse/Doppler are (+), time to redirect your attention away from acute arterial occlusion toward the:
🔵 Venous system
🔵 Microscopic vasculature (ie arterioles, capillaries, venules)
To tease out which system is at play, ask yourself question #2:
2) Is there a DVT?
 (View Tweet)
(View Tweet)
- If an extensive DVT is present, you may be dealing with ischemia due to compromise of the large venous vessels, leading to a non-gangrenous, reversible condition:
🔵 Phlegmasia Cerulea Dolens
- Patients with Phlegmasia classically have a painful, blue, swollen leg
 (View Tweet)
(View Tweet)
- If untreated, Phlegmasia may irreversibly progress to Venous Limb Gangrene ☠️
Some quick points on DVT-associated limb ischemia:
🔵 Classically, symptoms are unilateral & ipsilateral to the DVT
 (View Tweet)
(View Tweet)
- 🔵 If discovered, you should also consider the driver of DVT formation, because DIC is often at play. Common drivers include:
- 💊 Warfarin use must also be considered, as warfarin is often implicated in Venous Limb Gangrene
💊 Of note, "Warfarin skin necrosis" is a distinct entity involving primarily the skin, whereas Venous Limb Gangrene often involves deeper tissues (ie ↑ amputation risk)
 (View Tweet)
(View Tweet)
- Back to our schema!
🔍 If the patient does not have a DVT, your focus is now on microscopic vascular occlusion 🔍
Before diving into our endpoint diagnoses, let's review 2 related, "can't miss," DIC-related syndromes:
🔴 Symmetric Peripheral Gangrene
🔴 Purpura Fulminans
 (View Tweet)
(View Tweet)
- Symmetric Peripheral Gangrene (SPG) & Purpura Fulminans (PF) are typically seen in shock patients with ↓ platelets & coagulopathy
🔴 Symmetric, distal ("acral") necrosis = Symmetric Peripheral Gangrene
🔴 Non-acral, multicentric, extensive necrosis = Purpura Fulminans

 (View Tweet)
(View Tweet)
- ⚪ Pearl: preceding shock liver is seen in ~90% of patients who develop Symmetric Peripheral Gangrene!
- Skin findings usually begin 2-5 days after the initial transaminase elevation
- This time period may reflect the time needed for critical depletion of protein C levels
 (View Tweet)
(View Tweet)
- After considering SPG & PF, etiologies of "DVT-negative" Ischemic Limb Syndromes can be clustered:
"What can plug a microscopic vessel?"
👇
- Clots
- Emboli
- Proteins
- Inflammation
- Infections
- Crystals
Let's review a few endpoint diagnoses...
 (View Tweet)
(View Tweet)
- Emboli 💦
- SEPTIC: while the Osler nodes of infective endocarditis (IE) are pathognomonic, eponymic findings are actually less common
⚪ Of the <10% of IE patients with skin findings, purpura is most common & seen in ~8%! Extensive necrosis may be seen!
 (View Tweet)
(View Tweet)
- Proteins 🟢
- TYPE 1 CRYO: skin findings are seen in ~70-85% due to monoclonal cryoglobulin precipitation → purpura, livedo reticularis → ulceration
 (View Tweet)
(View Tweet)
-
- CRYOFIBRINOGENEMIA: cold-induced fibrin/fibrinogen precipitation → presentation similar to Type 1 cryo
- PARAPROTEINEMIAS: purpura can be seen in myeloma & Waldenstrom's due to non-cryoglobulinemic Ig deposits
 (View Tweet)
(View Tweet)
- Inflammation 🔥
- A number of SMALL/MEDIUM-vessel vasculitides can occlude the microvasculature, & isolated skin involvement can be seen in cutaneous small-vessel vasculitis
- THROMBOANGIITIS OBLITERANS: think young smokers with digital ulceration/gangrene
 (View Tweet)
(View Tweet)
- Some final helpful notes 📚
⚪ The purpura in these etiologies are frequently described as "retiform." This refers to a branched appearance of the dark red/purple purpuric lesions & signifies complete occlusion of the skin's microscopic vessels
 (View Tweet)
(View Tweet)
- ⚪ Livedoid vasculopathy: refers to skin biopsy showing microvascular thrombosis, endothelial proliferation, & subintimal hyaline degeneration → "livedoid changes" → ulceration. This is often secondary to pro-thrombotic disorders & rheumatic diseases!
 (View Tweet)
(View Tweet)
- ⚪ Since each endpoint Dx can manifest with "retiform" purpura (potentially progressing to ulceration/necrosis), how can you make diagnostic progress? Consider the following:
- Time course
- Distribution (eg acral vs. non-acral)
- Extra-dermatologic involvement
 (View Tweet)
(View Tweet)
- ⚪ Finally, consider mimickers!
🎭 Necrotizing skin/soft tissue infections (SSTIs)
🎭 Neutrophilic dermatoses
🎭 Trauma-related etiologies
(Note: there is some overlapping pathophys w/ the buckets of the "DVT-negative" list, but we've included this separately for simplicity.)
 (View Tweet)
(View Tweet)
- Before our 🏁 Takeaways 🏁 please give @OmarosisFugax a follow.
This schema & thread were co-created with Omar via numerous iterations behind-the-scenes. It simply wouldn't be the same w/o him & I'm so glad we collaborated. (View Tweet)
- 🏁 Takeaways
- If concern for an Ischemic Limb Syndrome (ie extremity pain + skin changes), first look for Pulse/Doppler signal, then consider DVT
- If pulses are (+) & there's no DVT, consider microvascular occlusion
- Prioritize SPG & PF in critically ill patients!
 (View Tweet)
(View Tweet)
- Save this schema on Glass (@GlassHealthHQ) here!
https://t.co/ONb8q4RUpd (View Tweet)
- References:
- https://t.co/pW9lCZiTFM
- https://t.co/PIEQ09uDAz
- https://t.co/c42nqgdVNS
- https://t.co/J0D0vq1gaa
- https://t.co/8uFxGAKcrZ
- https://t.co/zPZ66cEVEz
- https://t.co/b3a9PVq0yS
- https://t.co/EdfL9wTxvb (View Tweet)
- CC: @rabihmgeha @DxRxEdu @Sharminzi @AndreMansoor @rav7ks @KirtanPatolia @Rafameed @MadellenaC @Marcelaaos @AnnaFretz @ShreyaTrivediMD @AdamJBrownMD @medpedshosp @DrDanRestrepo @nsrosenberg @dereckwpaul @NazliDizman @MatthewHoMD @adil_rashidk @haematognomist @HannahRAbrams (View Tweet)
- @preardon @YaleIM_Chiefs @MarkDSiegel1 @Dr_AmerZeidan @ElizabethPrsic @tony_breu @DoctorWatto @PaulNWilliamz @Sofiacruzsolbes @RMadhavanMD @Heard_that_alex @SJMagierMD @ana_ferrigno @AnnSolimanMD @PulmCrit @AaronGoodman33 @LandsbergManual
@TheRealDSrini @DruvBhagavan
@PBlivenMD (View Tweet)

 (View Tweet)
(View Tweet)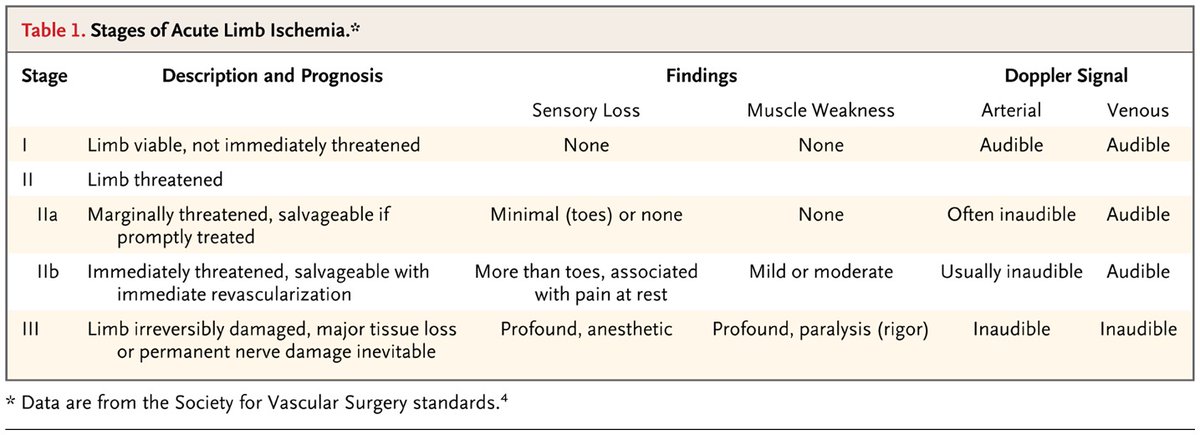
 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)
 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)
 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)